Monkeypox is a large DNA virus belonging to the orthopoxvirus family. There have been more than 4,100 confirmed cases globally.
The World Health Organisation (WHO) has decided not to declare monkeypox a public health emergency of international concern as of now.
However, WHO Director-General Tedros Adhanom Ghebreyesus said he was deeply concerned about the evolving threat of monkeypox, which he said had reached more than 50 countries.
There have been more than 4,100 confirmed cases globally, including at least 13 in Australia. The WHO also acknowledged there were many unknowns about the outbreak.
What is Monkeypox?
Monkeypox is a large DNA virus belonging to the orthopoxvirus family. Unlike the related smallpox virus, variola, which only affected humans, monkeypox virus is found in rodents and other animals in parts of Africa.
We know of two clades (virus groupings), and it is the less severe of the two currently circulating outside Africa.
Orthopoxviruses are stable viruses that do not mutate much. Multiple mutations, however, have been described in the virus causing the current outbreak.
In the United States, at least two separate strains have been circulating, suggesting multiple introductions into the country.
How far will it spread? Does COVID make a difference?
Does the COVID pandemic increase the risk? Possibly, yes. Due to waning immunity from the smallpox vaccine globally and the spread of monkeypox to many countries already, we may see the epidemic spreading more widely.
If it does so and starts infecting large numbers of children, we could see more deaths because children get a more severe infection.
So, we should monitor globally for clusters of fever and rash, and misdiagnosis as chickenpox, hand foot and mouth disease, herpes simplex or other diseases with a rash.
Another factor is COVID-19. As people recover from Covid, their immune system is impaired. So, people who have had Covid may be more susceptible to other infections.
We see the same with measles infection. This weakens the immune system and increases the risk of other infections for two to three years afterwards.
If the epidemic becomes established in countries outside the endemic areas, it may infect animals and create new endemic zones in the world. It is important we do everything possible to stop this epidemic.
READ | Stampede or mass poisoning? 21 teens die in South African nightclub under ‘mysterious circumstances’
Vaccines and treatments
Past vaccination against smallpox provides 85% protection against monkeypox. Smallpox was declared eradicated in 1980, so most mass vaccination programs ceased in the 1970s.
Australia never had mass smallpox vaccination. However, an estimated 10% of Australians have been vaccinated in the past, mostly migrants.
Vaccines protect for many years but immunity wanes. So declining population-level protection is likely responsible for the resurgence of monkeypox seen since 2017 in Nigeria, one of seven endemic hot spots in Africa.
Mass vaccination is not recommended. But vaccines can be given to contacts of confirmed cases (known as post-exposure prophylaxis) and people at high risk of contracting the virus, such as some lab or health workers (pre-exposure prophylaxis).
There are also treatments, such as vaccinia immune globulin and antivirals. These were developed against smallpox.
(With inputs from PTI)
![submenu-img]() Weather update: IMD predicts light to moderate rain, thunderstorms in Delhi-NCR; check forecast here
Weather update: IMD predicts light to moderate rain, thunderstorms in Delhi-NCR; check forecast here![submenu-img]() 'I can't breathe': Black man in Ohio pleads as police officers pin him to floor, then...
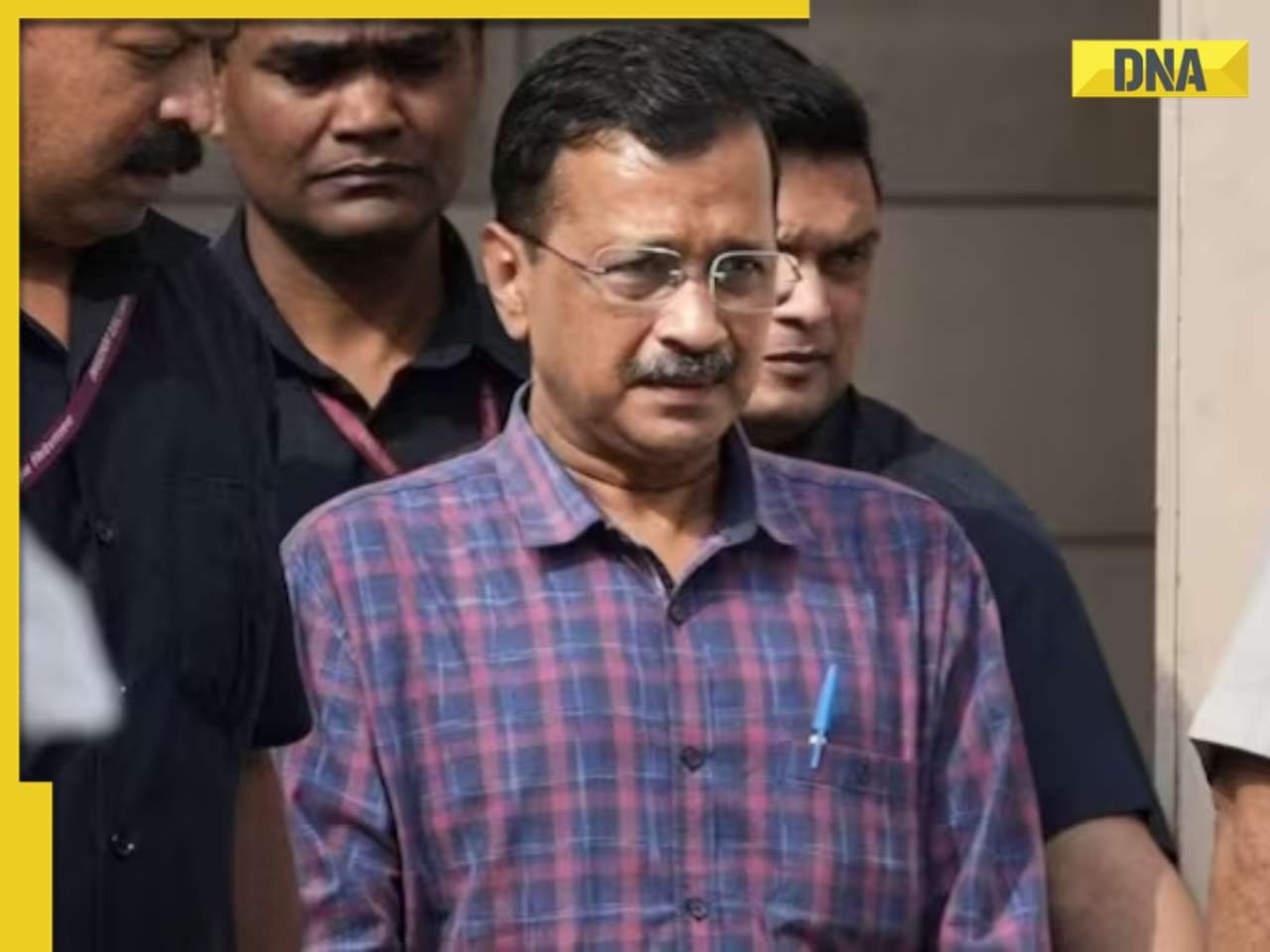
'I can't breathe': Black man in Ohio pleads as police officers pin him to floor, then...![submenu-img]() Delhi HC raps CM Kejriwal, accuses him of prioritising political interest by continuing as CM after arrest
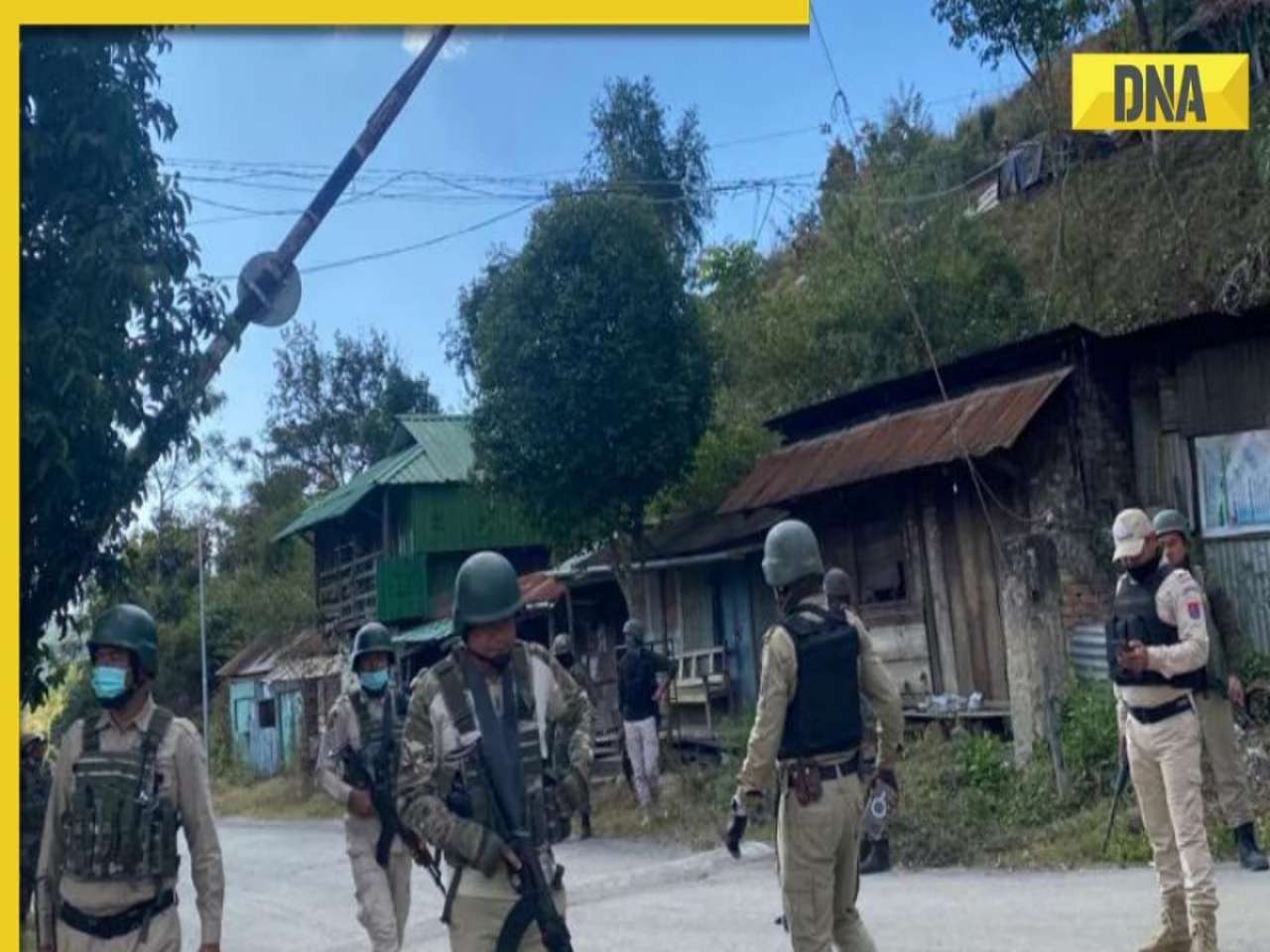
Delhi HC raps CM Kejriwal, accuses him of prioritising political interest by continuing as CM after arrest![submenu-img]() Manipur: Two CRPF personnel killed in Kuki militants' attack in Naransena area
Manipur: Two CRPF personnel killed in Kuki militants' attack in Naransena area![submenu-img]() These 9 Indian dishes make it to the list of ‘best stews in the world’
These 9 Indian dishes make it to the list of ‘best stews in the world’![submenu-img]() DNA Verified: Is CAA an anti-Muslim law? Centre terms news report as 'misleading'
DNA Verified: Is CAA an anti-Muslim law? Centre terms news report as 'misleading'![submenu-img]() DNA Verified: Lok Sabha Elections 2024 to be held on April 19? Know truth behind viral message
DNA Verified: Lok Sabha Elections 2024 to be held on April 19? Know truth behind viral message![submenu-img]() DNA Verified: Modi govt giving students free laptops under 'One Student One Laptop' scheme? Know truth here
DNA Verified: Modi govt giving students free laptops under 'One Student One Laptop' scheme? Know truth here![submenu-img]() DNA Verified: Shah Rukh Khan denies reports of his role in release of India's naval officers from Qatar
DNA Verified: Shah Rukh Khan denies reports of his role in release of India's naval officers from Qatar![submenu-img]() DNA Verified: Is govt providing Rs 1.6 lakh benefit to girls under PM Ladli Laxmi Yojana? Know truth
DNA Verified: Is govt providing Rs 1.6 lakh benefit to girls under PM Ladli Laxmi Yojana? Know truth![submenu-img]() In pics: Arti Singh stuns in red lehenga as she ties the knot with beau Dipak Chauhan in dreamy wedding
In pics: Arti Singh stuns in red lehenga as she ties the knot with beau Dipak Chauhan in dreamy wedding![submenu-img]() Actors who died due to cosmetic surgeries
Actors who died due to cosmetic surgeries![submenu-img]() See inside pics: Malayalam star Aparna Das' dreamy wedding with Manjummel Boys actor Deepak Parambol
See inside pics: Malayalam star Aparna Das' dreamy wedding with Manjummel Boys actor Deepak Parambol ![submenu-img]() In pics: Salman Khan, Alia Bhatt, Rekha, Neetu Kapoor attend grand premiere of Sanjay Leela Bhansali's Heeramandi
In pics: Salman Khan, Alia Bhatt, Rekha, Neetu Kapoor attend grand premiere of Sanjay Leela Bhansali's Heeramandi![submenu-img]() Streaming This Week: Crakk, Tillu Square, Ranneeti, Dil Dosti Dilemma, latest OTT releases to binge-watch
Streaming This Week: Crakk, Tillu Square, Ranneeti, Dil Dosti Dilemma, latest OTT releases to binge-watch![submenu-img]() DNA Explainer: Why Harvey Weinstein's rape conviction was overturned, will beleaguered Hollywood mogul get out of jail?
DNA Explainer: Why Harvey Weinstein's rape conviction was overturned, will beleaguered Hollywood mogul get out of jail?![submenu-img]() What is inheritance tax?
What is inheritance tax?![submenu-img]() DNA Explainer: What is cloud seeding which is blamed for wreaking havoc in Dubai?
DNA Explainer: What is cloud seeding which is blamed for wreaking havoc in Dubai?![submenu-img]() DNA Explainer: What is Israel's Arrow-3 defence system used to intercept Iran's missile attack?
DNA Explainer: What is Israel's Arrow-3 defence system used to intercept Iran's missile attack?![submenu-img]() DNA Explainer: How Iranian projectiles failed to breach iron-clad Israeli air defence
DNA Explainer: How Iranian projectiles failed to breach iron-clad Israeli air defence![submenu-img]() Krishna Mukherjee accuses Shubh Shagun producer of harassing, threatening her: ‘I was changing clothes when...'
Krishna Mukherjee accuses Shubh Shagun producer of harassing, threatening her: ‘I was changing clothes when...'![submenu-img]() Meet 90s top Bollywood actress, who gave hits with Shah Rukh, Salman, Aamir, one mistake ended career; has now become…
Meet 90s top Bollywood actress, who gave hits with Shah Rukh, Salman, Aamir, one mistake ended career; has now become…![submenu-img]() This actress, who once worked as pre-school teacher, changed diapers, later gave six Rs 100-crore films; is now worth…
This actress, who once worked as pre-school teacher, changed diapers, later gave six Rs 100-crore films; is now worth…![submenu-img]() 'There were days when I didn't want to probably live': Adhyayan Suman opens up on rough patch in his career
'There were days when I didn't want to probably live': Adhyayan Suman opens up on rough patch in his career![submenu-img]() This low-budget film with no star is 2024's highest-grossing Indian film; beat Fighter, Shaitaan, Bade Miyan Chote Miyan
This low-budget film with no star is 2024's highest-grossing Indian film; beat Fighter, Shaitaan, Bade Miyan Chote Miyan![submenu-img]() World wrestling body threatens to reimpose ban on WFI if...
World wrestling body threatens to reimpose ban on WFI if...![submenu-img]() IPL 2024: Jonny Bairstow, Shashank Singh special power Punjab Kings to record run-chase against KKR
IPL 2024: Jonny Bairstow, Shashank Singh special power Punjab Kings to record run-chase against KKR![submenu-img]() DC vs MI, IPL 2024: Predicted playing XI, live streaming details, weather and pitch report
DC vs MI, IPL 2024: Predicted playing XI, live streaming details, weather and pitch report![submenu-img]() DC vs MI IPL 2024 Dream11 prediction: Fantasy cricket tips for Delhi Capitals vs Mumbai Indians
DC vs MI IPL 2024 Dream11 prediction: Fantasy cricket tips for Delhi Capitals vs Mumbai Indians![submenu-img]() Yuvraj Singh named ICC Men's T20 World Cup 2024 Ambassador
Yuvraj Singh named ICC Men's T20 World Cup 2024 Ambassador![submenu-img]() Watch: Lioness teaches cubs to climb tree, adorable video goes viral
Watch: Lioness teaches cubs to climb tree, adorable video goes viral![submenu-img]() Viral video: Little girl's impressive lion roar wins hearts on internet, watch
Viral video: Little girl's impressive lion roar wins hearts on internet, watch![submenu-img]() Who is Sangeet Singh? Man arrested for posing as Singapore Airlines pilot at Delhi airport
Who is Sangeet Singh? Man arrested for posing as Singapore Airlines pilot at Delhi airport![submenu-img]() One of India’s most expensive wedding, attended by 5000 people, 100 room villa, cost Rs…
One of India’s most expensive wedding, attended by 5000 people, 100 room villa, cost Rs…![submenu-img]() Viral video: Delhi's 'Spiderman' take to streets on bike, get arrested; watch
Viral video: Delhi's 'Spiderman' take to streets on bike, get arrested; watch





































)




)
)
)
)
)
)