General and health insurance companies launched the "Cashless Everywhere" initiative in partnership with the General Insurance Council.
There's a new change in the Indian medical industry. People can now pay for their medical care at any hospital in the country with cashless options. This follows the decision made by general and health insurance companies to provide medical insurance policyholders with 100% cashless treatment starting on Thursday, January 25.
General and health insurance companies launched the "Cashless Everywhere" initiative in partnership with the General Insurance Council, the highest authority for general insurers.
What's the current guidelines?
With a cashless facility, policyholders are not required to pay for hospital treatment under the terms of their current health insurance policies. Instead, insurance companies agree to pay for hospital treatment as long as the claim is accepted.
There are only a few hospitals that offer this cashless service due to agreements or partnerships with the individual insurance company. The policyholder will not be able to access this facility, though, if he selects a different hospital without a signed agreement. In that scenario, the client will need to file a reimbursement claim, which will cause the claim procedure to be further delayed.
About the new medical policy guidelines
However, under the new programme, policyholders can receive care at any hospital—regardless of whether the facility is part of the insurance company's network—for free. According to Indian Express, it enables the policyholder to be admitted to any hospital of their choice without having to pay a deposit up front, with insurance companies paying the balance on the day of discharge.
According to this, the policyholder must notify the insurance provider at least 48 hours in advance of admission. If the policyholder needs emergency care, they have 48 hours from the time of admission to notify the insurance company.
According to the General Insurance Council,“The claim should be admissible as per the terms of the policy and the cashless facility should be admissible as per the operating guidelines of the insurance company."
![submenu-img]() Weather update: IMD predicts light to moderate rain, thunderstorms in Delhi-NCR; check forecast here
Weather update: IMD predicts light to moderate rain, thunderstorms in Delhi-NCR; check forecast here![submenu-img]() 'I can't breathe': Black man in Ohio pleads as police officers pin him to floor, then...
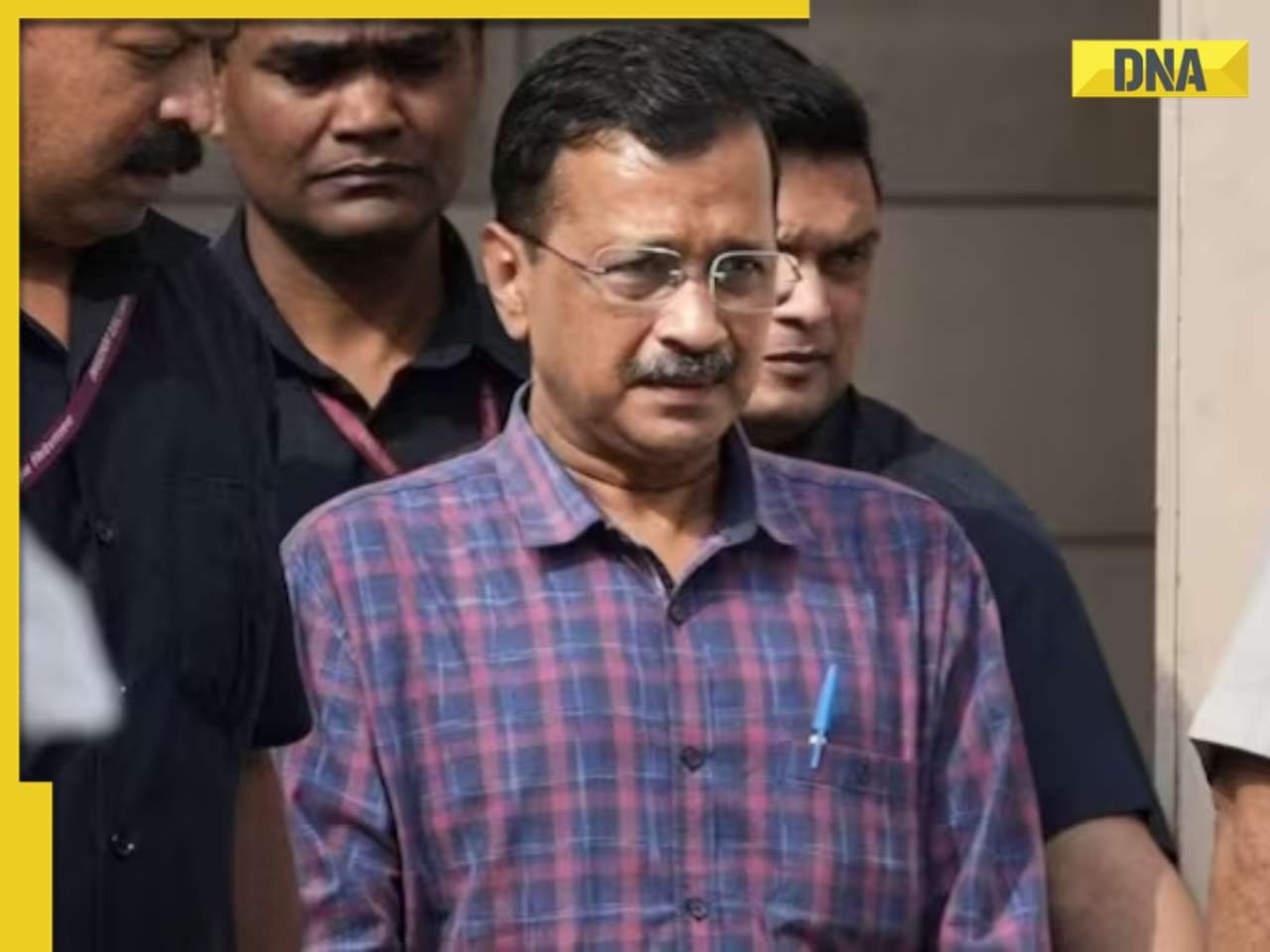
'I can't breathe': Black man in Ohio pleads as police officers pin him to floor, then...![submenu-img]() Delhi HC raps CM Kejriwal, accuses him of prioritising political interest by continuing as CM after arrest
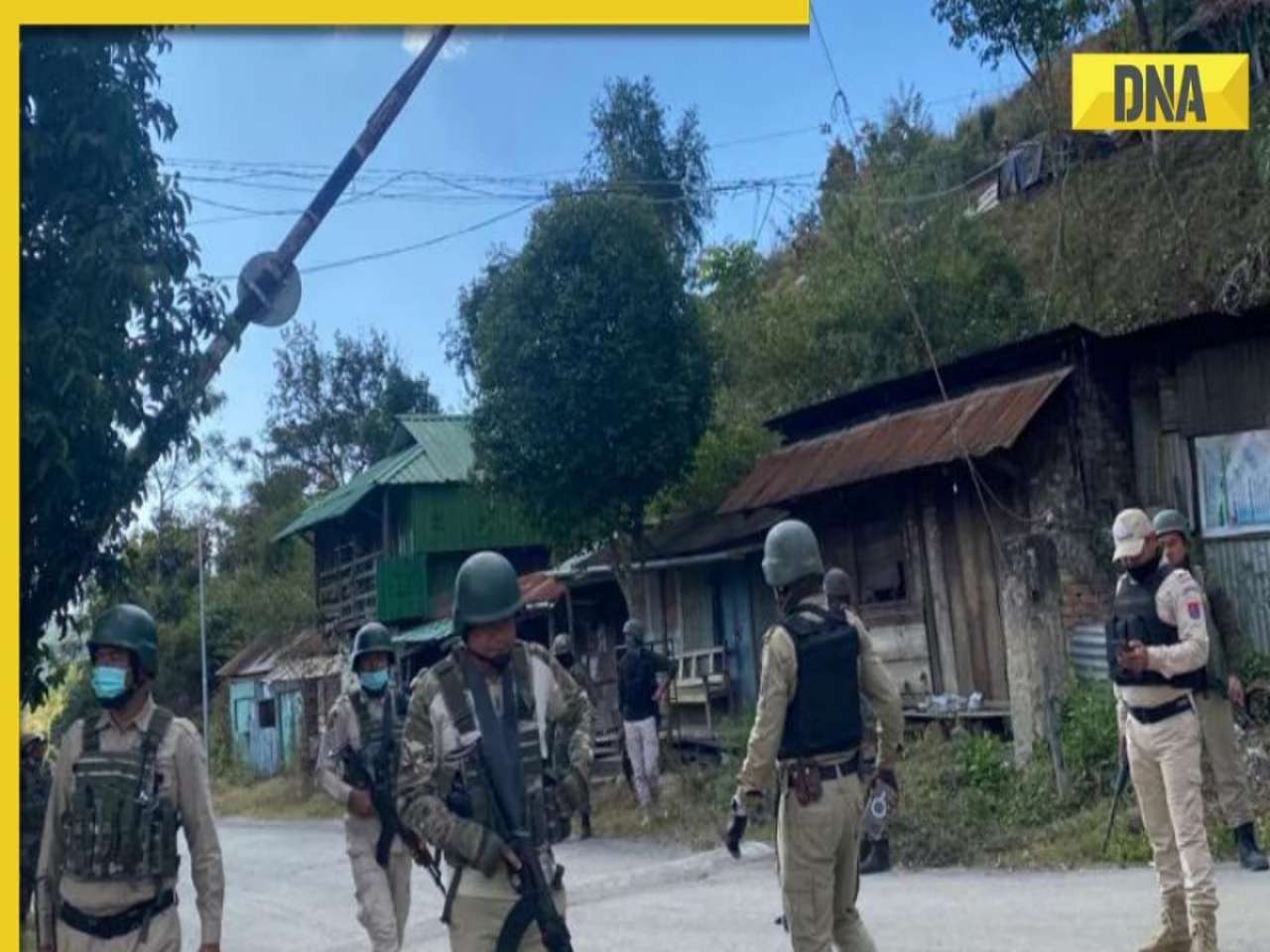
Delhi HC raps CM Kejriwal, accuses him of prioritising political interest by continuing as CM after arrest![submenu-img]() Manipur: Two CRPF personnel killed in Kuki militants' attack in Naransena area
Manipur: Two CRPF personnel killed in Kuki militants' attack in Naransena area![submenu-img]() These 9 Indian dishes make it to the list of ‘best stews in the world’
These 9 Indian dishes make it to the list of ‘best stews in the world’![submenu-img]() DNA Verified: Is CAA an anti-Muslim law? Centre terms news report as 'misleading'
DNA Verified: Is CAA an anti-Muslim law? Centre terms news report as 'misleading'![submenu-img]() DNA Verified: Lok Sabha Elections 2024 to be held on April 19? Know truth behind viral message
DNA Verified: Lok Sabha Elections 2024 to be held on April 19? Know truth behind viral message![submenu-img]() DNA Verified: Modi govt giving students free laptops under 'One Student One Laptop' scheme? Know truth here
DNA Verified: Modi govt giving students free laptops under 'One Student One Laptop' scheme? Know truth here![submenu-img]() DNA Verified: Shah Rukh Khan denies reports of his role in release of India's naval officers from Qatar
DNA Verified: Shah Rukh Khan denies reports of his role in release of India's naval officers from Qatar![submenu-img]() DNA Verified: Is govt providing Rs 1.6 lakh benefit to girls under PM Ladli Laxmi Yojana? Know truth
DNA Verified: Is govt providing Rs 1.6 lakh benefit to girls under PM Ladli Laxmi Yojana? Know truth![submenu-img]() In pics: Arti Singh stuns in red lehenga as she ties the knot with beau Dipak Chauhan in dreamy wedding
In pics: Arti Singh stuns in red lehenga as she ties the knot with beau Dipak Chauhan in dreamy wedding![submenu-img]() Actors who died due to cosmetic surgeries
Actors who died due to cosmetic surgeries![submenu-img]() See inside pics: Malayalam star Aparna Das' dreamy wedding with Manjummel Boys actor Deepak Parambol
See inside pics: Malayalam star Aparna Das' dreamy wedding with Manjummel Boys actor Deepak Parambol ![submenu-img]() In pics: Salman Khan, Alia Bhatt, Rekha, Neetu Kapoor attend grand premiere of Sanjay Leela Bhansali's Heeramandi
In pics: Salman Khan, Alia Bhatt, Rekha, Neetu Kapoor attend grand premiere of Sanjay Leela Bhansali's Heeramandi![submenu-img]() Streaming This Week: Crakk, Tillu Square, Ranneeti, Dil Dosti Dilemma, latest OTT releases to binge-watch
Streaming This Week: Crakk, Tillu Square, Ranneeti, Dil Dosti Dilemma, latest OTT releases to binge-watch![submenu-img]() DNA Explainer: Why Harvey Weinstein's rape conviction was overturned, will beleaguered Hollywood mogul get out of jail?
DNA Explainer: Why Harvey Weinstein's rape conviction was overturned, will beleaguered Hollywood mogul get out of jail?![submenu-img]() What is inheritance tax?
What is inheritance tax?![submenu-img]() DNA Explainer: What is cloud seeding which is blamed for wreaking havoc in Dubai?
DNA Explainer: What is cloud seeding which is blamed for wreaking havoc in Dubai?![submenu-img]() DNA Explainer: What is Israel's Arrow-3 defence system used to intercept Iran's missile attack?
DNA Explainer: What is Israel's Arrow-3 defence system used to intercept Iran's missile attack?![submenu-img]() DNA Explainer: How Iranian projectiles failed to breach iron-clad Israeli air defence
DNA Explainer: How Iranian projectiles failed to breach iron-clad Israeli air defence![submenu-img]() Krishna Mukherjee accuses Shubh Shagun producer of harassing, threatening her: ‘I was changing clothes when...'
Krishna Mukherjee accuses Shubh Shagun producer of harassing, threatening her: ‘I was changing clothes when...'![submenu-img]() Meet 90s top Bollywood actress, who gave hits with Shah Rukh, Salman, Aamir, one mistake ended career; has now become…
Meet 90s top Bollywood actress, who gave hits with Shah Rukh, Salman, Aamir, one mistake ended career; has now become…![submenu-img]() This actress, who once worked as pre-school teacher, changed diapers, later gave six Rs 100-crore films; is now worth…
This actress, who once worked as pre-school teacher, changed diapers, later gave six Rs 100-crore films; is now worth…![submenu-img]() 'There were days when I didn't want to probably live': Adhyayan Suman opens up on rough patch in his career
'There were days when I didn't want to probably live': Adhyayan Suman opens up on rough patch in his career![submenu-img]() This low-budget film with no star is 2024's highest-grossing Indian film; beat Fighter, Shaitaan, Bade Miyan Chote Miyan
This low-budget film with no star is 2024's highest-grossing Indian film; beat Fighter, Shaitaan, Bade Miyan Chote Miyan![submenu-img]() World wrestling body threatens to reimpose ban on WFI if...
World wrestling body threatens to reimpose ban on WFI if...![submenu-img]() IPL 2024: Jonny Bairstow, Shashank Singh special power Punjab Kings to record run-chase against KKR
IPL 2024: Jonny Bairstow, Shashank Singh special power Punjab Kings to record run-chase against KKR![submenu-img]() DC vs MI, IPL 2024: Predicted playing XI, live streaming details, weather and pitch report
DC vs MI, IPL 2024: Predicted playing XI, live streaming details, weather and pitch report![submenu-img]() DC vs MI IPL 2024 Dream11 prediction: Fantasy cricket tips for Delhi Capitals vs Mumbai Indians
DC vs MI IPL 2024 Dream11 prediction: Fantasy cricket tips for Delhi Capitals vs Mumbai Indians![submenu-img]() Yuvraj Singh named ICC Men's T20 World Cup 2024 Ambassador
Yuvraj Singh named ICC Men's T20 World Cup 2024 Ambassador![submenu-img]() Watch: Lioness teaches cubs to climb tree, adorable video goes viral
Watch: Lioness teaches cubs to climb tree, adorable video goes viral![submenu-img]() Viral video: Little girl's impressive lion roar wins hearts on internet, watch
Viral video: Little girl's impressive lion roar wins hearts on internet, watch![submenu-img]() Who is Sangeet Singh? Man arrested for posing as Singapore Airlines pilot at Delhi airport
Who is Sangeet Singh? Man arrested for posing as Singapore Airlines pilot at Delhi airport![submenu-img]() One of India’s most expensive wedding, attended by 5000 people, 100 room villa, cost Rs…
One of India’s most expensive wedding, attended by 5000 people, 100 room villa, cost Rs…![submenu-img]() Viral video: Delhi's 'Spiderman' take to streets on bike, get arrested; watch
Viral video: Delhi's 'Spiderman' take to streets on bike, get arrested; watch





































)




)
)
)
)
)
)