
With lifestyle changes, disease patterns have also changed. Coronary artery diseases, knee joint problems and other lifestyle ailments are on the rise. New technologies have offered remedies to many of these new diseases.
These technologies require more funding to meet the needs of our population. But unfortunately, public spending on health has not increased proportionately; instead there was a reduction in the health budget by about 20 per cent in 2015. With the government shedding its responsibility, most new healthcare facilities have emerged in the corporate sector — unaffordable to a vast majority of our population. With the paradigm shift in approach towards health from a social responsibility to purchasable commodity since the early 1990s, the race to profiteer — right from the manufacturers, middlemen, to health providers — has become an integral part of this system. It is disturbing to note that over four crore people in our country enter the below poverty line (BPL) category every year, because of out-of-pocket expenditure on health.
Drugs and consumables account for 67 per cent of healthcare costs. The National Pharmaceutical Pricing Authority (NPPA) has in the past demarcated essential drugs and brought them under the Drug Price Control Order (DPCO). Despite being only 12 per cent of the total medicines, this gave relief to the end-users. The NPPA has now very rightly taken cognisance of the price of the stents and has started consultation with various stakeholders, the industry, cardiologists, medical organisations and civil society groups so as to formulate a policy on capping the price of the coronary stents.
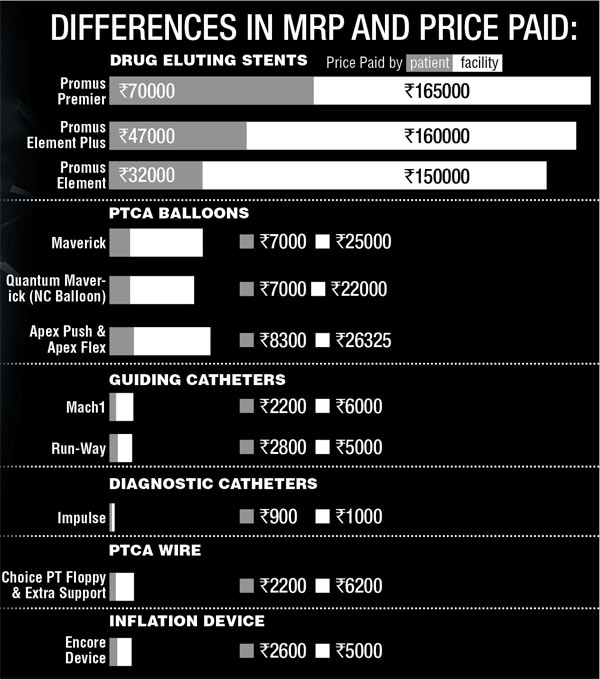
Angioplasty and stenting are lifesaving procedures. There are several types of stents depending on their size and other features. The bare metal stents have now been replaced largely by the drug eluting second-generation stents. It is imperative that they are made available at low cost. But after passing through the supply chain: the importer, stockist, and the middleman selling to the healthcare facility their cost increases to 700 - 800 per cent. It is obvious from the table (above) that there is a huge price difference between the amount charged from patients (the Maximum Retail Price) and the price at which the facility purchases from the seller. In this case, the facility may be the institution or sometimes the cardiologist directly. Whereas the cost increases at every step in the supply chain, it has been revealed that maximum rise in the cost occurs in the last step where the facility inserts the stent. With such exorbitant profit there is always a scope of unhealthy medical practices coupled with greed.
The NPPA has taken up a big challenge to cap these prices. We from the Alliance of Doctors for Ethical Health Care (ADEH) have put several suggestions to the Chairman of the NPPA which could help in controlling the price to the end user.
The cost must be capped in the manufacturing stage. It should be calculated on the basis of cost accountancy which means actual money spent in their production. The profit margin on these should not be more than 20 per cent by the time it reaches the end user. The manufacturers should put the details of their products on the website along with its cost. The price of each stent should be displayed at the reception counter of the facility putting stents. The patient deserves the options with a full scientific explanation. He/she should be free to purchase stents from the market. The present policy of packages is not transparent about exactly how much is spent on the stent vs other services. A separate bill for the stent can help with this. The persons inserting stents should charge their own fee only without profit. There should be regular financial, clinical and medical audit of such facilities.
Indigenous production should be encouraged and facilitated with international quality control; till then import duty and other taxes should be waived off. Any difference between the new types of stents should be evaluated by experts from reputed cardiac centers like AIIMS and PGI. Now this evaluation is done by the companies who disseminate information on the quality differences through their representatives.
Ethics must be supreme. No wonder big companies spend huge amount on giving freebies to the medical professionals which even includes foreign travel. Most of the academic conferences are sponsored by the pharmaceutical giants. This practice has to be shunned. Laws have to be amended accordingly. The present code of conduct for doctors prohibits them from accepting any considerations from the companies but this does not apply to organisations. The Uniform Code of Pharmaceutical Marketing Practices which asks the companies to refrain from giving such grants to the doctors is voluntary so far. It has to be made mandatory.
The NPPA has taken up a big challenge which is likely to meet resistance from the industry, the dealers, the facilities putting stents and a section of the doctors. However, sensitive doctors and concerned citizens have great expectations from the NPPA on regulating the pricing of stents. Similar anomalies also exist in the pricing of drugs, including generic drugs where too there is a huge difference between the cost and the MRP. The NPPA has its task cut out.
The author is an ENT surgeon and a former chairman of the Punjab Medical Council’s Ethics Committee