Dr Kenneth Thorpe, chairman, US-based 'The Partnership to Fight Chronic Disease' (PFCD) in conversation with Maitri Porecha on his advise to the Modi government about non-communicable diseases (NCDs) posing the single greatest threat to India's health
What is the need of a blueprint to tackle NCDs in India?
There are fragmented elements but no comprehensive plan. India has 6.5 crore diabetics and it is estimated that the number will rise to 12 crore over the next decade. Unless some interventions are put in place now, things will only go downhill. It has been observed that this spike is related to an increase in income and changing eating patterns in countries. People have resorted to having packaged food, rather than consuming indigenous meals. Globally, the price of processed food has become very cheap and is available at a low price for people having time constraints.
A national blueprint will harness some of the best thinkers by roping in patient advocacy groups and experts. Up to five or six NCDs can ail a person at one go. A person may suffer from high blood pressure, obesity, high cholesterol, asthma and depression at once. A clinician may focus on controlling blood pressure, but may not know have to treat depression. A blueprint will aid us in managing all of these entirely.
Since when did the PFCD start engaging, previously with the UPA govt, and now, with the BJP-led NDA govt, to propose a national blueprint plan for tackling NCDs in India?
We started engaging with the Indian govt since almost five years. There was no positive response initially and lots of problems had arisen, including finger-pointing. But lately, things have started to look brighter and there is hope that under the current govt, a blueprint will come through.
Why has there not been a national blueprint in place to tackle NCDs till date?
There is substantial shortage of manpower. The problem of NCDs is widespread, but there is little investment to tackle it. Budget allocated for health is barely 4%-5% of the gross domestic product (GDP). Thus, the gap between needs and investment is very substantial. Unless we do something now, 10 – 15 years down the line, things are set to get worse.\
What have you proposed that India considers while developing a blueprint?
Developing a blueprint or a road map will entail a five-pronged approach. We have proposed that the focus be on ways to prevent the growth of NCDs by looking into international prevention programs. Also, there should be mechanisms to increase detection and screening rates. Further, we should look at how to best deliver services and manage patients that are suffering from five to six chronic conditions simultaneously. Financing programmes is priority. Health insurance should be made available for chronic disease management. Infectious and non-infectious diseases are interrelated and cross susceptibility risks are high, both should be managed together.
Which countries are highly susceptible and face the biggest challenges due to NCDs?
NCDs kill over 36 mn people each year. Nearly 80% of NCD-related deaths – 29 mn – occur in low and middle-income countries. Over 9 mn of all deaths attributed to NCDs occur before the age of 60; Cardiovascular diseases account for most NCD deaths, or 17.3 mn people annually, followed by cancer (7.6 million), respiratory diseases (4.2 million), and diabetes (1.3 million). In parts of Asia and Africa, NCDs like diabetes, blood pressure, stroke and heart attacks pose the biggest challenge. As much as 60% of mortality in a population is linked to NCDs. China has the highest burden of NCDs in the world with close to 8 crore people are suffering from diabetes.
In the US, are the NCDs on a rise or on a decline? Also, what role does health care reforms play in controlling NCDs?
In the 1960s, surveys indicated that up to 55% of adults smoked. This has reduced to less than half, with only 21%. This has led to controlling NCDs. There is a sharp reduction in cardiovascular deaths and stroke. Raising federal and state taxes on tobacco products and effective smoking cessation programs have made a huge difference to people's lives. Also, banning advertisements of tobacco products has changed the public and social view of smoking.
Only two things decide the passage or rejection of insurance claims in the US, whether you smoke or not, and your age. In India, health complications arising from diabetes and other chronic diseases are not included in health insurance. In the US, regulation of insurance is very strict, especially after the health care reforms act that was introduced in 2010. In India, the way the insurance schemes are designed, they mostly don't cover chronically ill patients. But in the US, claims don't get passed or rejected depending on how ill a person is.
Can you share success stories of effective prevention programs for NCDs across the world?
The diabetes prevention program that was implemented for over 15 years for 5,000 people in 30 communities across the US, is a striking example. It included people following a 16-week curriculum
where researchers sat down with people and helped them set up goals on nutritional and calorie components of their diet. It also included behaviour change modules including physical activity which compels one to stay physically active at least 150 minutes a week by walking, running, biking, jumping rope. The study was divided into three groups and was conducted in pre-diabetics who were overweight and had sugar levels edging towards being diabetic. The group with lifestyle intervention module had 58% lesser chances of becoming diabetic, as opposed to the placebo group. These programs were later replicated in Finland and China with much success.
![submenu-img]() First Bollywood star to wear bikini was called greatest actress ever, later isolated herself, died alone, her body was..
First Bollywood star to wear bikini was called greatest actress ever, later isolated herself, died alone, her body was..![submenu-img]() Apple iPhone camera module may now be assembled in India, plans to cut…
Apple iPhone camera module may now be assembled in India, plans to cut…![submenu-img]() HOYA Vision Care launches new hi-vision Meiryo coating
HOYA Vision Care launches new hi-vision Meiryo coating![submenu-img]() This film had no superstars, got slow start at box office, was made with budget of only Rs 60 lakh, earned Rs...
This film had no superstars, got slow start at box office, was made with budget of only Rs 60 lakh, earned Rs...![submenu-img]() Shocking details about 'Death Valley', one of the world's hottest places
Shocking details about 'Death Valley', one of the world's hottest places![submenu-img]() DNA Verified: Is CAA an anti-Muslim law? Centre terms news report as 'misleading'
DNA Verified: Is CAA an anti-Muslim law? Centre terms news report as 'misleading'![submenu-img]() DNA Verified: Lok Sabha Elections 2024 to be held on April 19? Know truth behind viral message
DNA Verified: Lok Sabha Elections 2024 to be held on April 19? Know truth behind viral message![submenu-img]() DNA Verified: Modi govt giving students free laptops under 'One Student One Laptop' scheme? Know truth here
DNA Verified: Modi govt giving students free laptops under 'One Student One Laptop' scheme? Know truth here![submenu-img]() DNA Verified: Shah Rukh Khan denies reports of his role in release of India's naval officers from Qatar
DNA Verified: Shah Rukh Khan denies reports of his role in release of India's naval officers from Qatar![submenu-img]() DNA Verified: Is govt providing Rs 1.6 lakh benefit to girls under PM Ladli Laxmi Yojana? Know truth
DNA Verified: Is govt providing Rs 1.6 lakh benefit to girls under PM Ladli Laxmi Yojana? Know truth![submenu-img]() In pics: Rajinikanth, Kamal Haasan, Mani Ratnam, Suriya attend S Shankar's daughter Aishwarya's star-studded wedding
In pics: Rajinikanth, Kamal Haasan, Mani Ratnam, Suriya attend S Shankar's daughter Aishwarya's star-studded wedding![submenu-img]() In pics: Sanya Malhotra attends opening of school for neurodivergent individuals to mark World Autism Month
In pics: Sanya Malhotra attends opening of school for neurodivergent individuals to mark World Autism Month![submenu-img]() Remember Jibraan Khan? Shah Rukh's son in Kabhi Khushi Kabhie Gham, who worked in Brahmastra; here’s how he looks now
Remember Jibraan Khan? Shah Rukh's son in Kabhi Khushi Kabhie Gham, who worked in Brahmastra; here’s how he looks now![submenu-img]() From Bade Miyan Chote Miyan to Aavesham: Indian movies to watch in theatres this weekend
From Bade Miyan Chote Miyan to Aavesham: Indian movies to watch in theatres this weekend ![submenu-img]() Streaming This Week: Amar Singh Chamkila, Premalu, Fallout, latest OTT releases to binge-watch
Streaming This Week: Amar Singh Chamkila, Premalu, Fallout, latest OTT releases to binge-watch![submenu-img]() DNA Explainer: What is Israel's Arrow-3 defence system used to intercept Iran's missile attack?
DNA Explainer: What is Israel's Arrow-3 defence system used to intercept Iran's missile attack?![submenu-img]() DNA Explainer: How Iranian projectiles failed to breach iron-clad Israeli air defence
DNA Explainer: How Iranian projectiles failed to breach iron-clad Israeli air defence![submenu-img]() DNA Explainer: What is India's stand amid Iran-Israel conflict?
DNA Explainer: What is India's stand amid Iran-Israel conflict?![submenu-img]() DNA Explainer: Why Iran attacked Israel with hundreds of drones, missiles
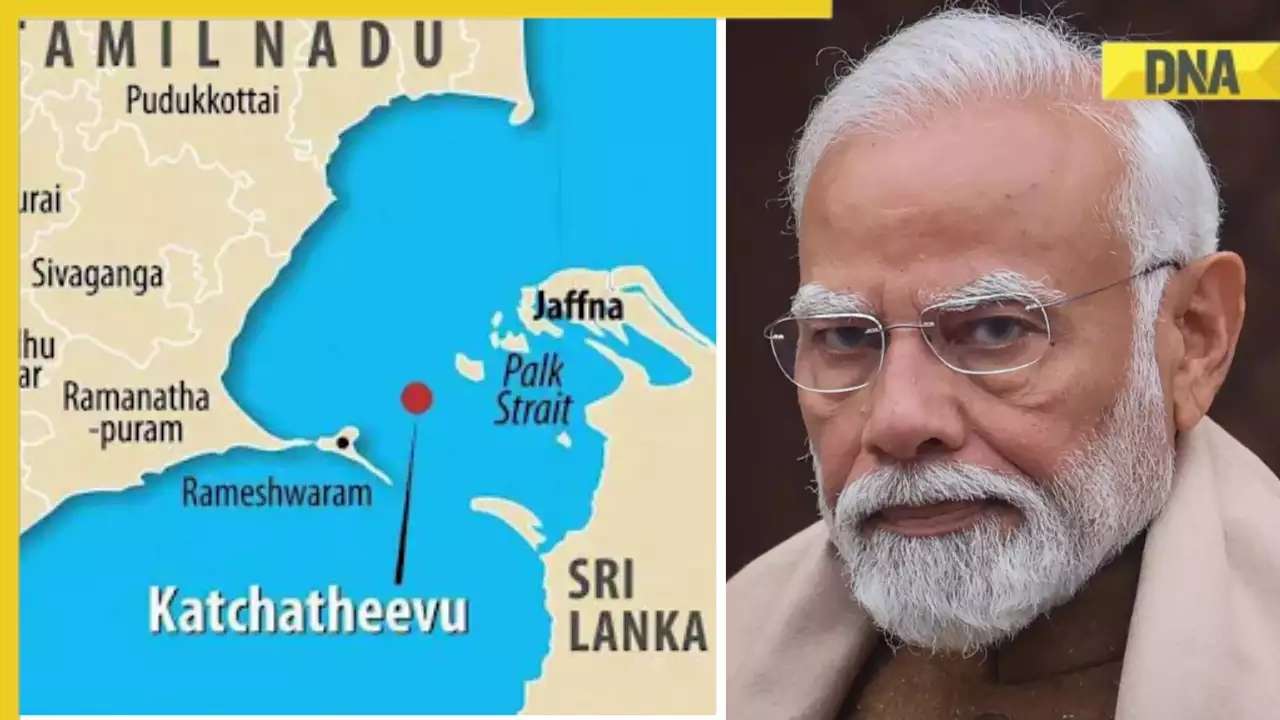
DNA Explainer: Why Iran attacked Israel with hundreds of drones, missiles![submenu-img]() What is Katchatheevu island row between India and Sri Lanka? Why it has resurfaced before Lok Sabha Elections 2024?
What is Katchatheevu island row between India and Sri Lanka? Why it has resurfaced before Lok Sabha Elections 2024?![submenu-img]() First Bollywood star to wear bikini was called greatest actress ever, later isolated herself, died alone, her body was..
First Bollywood star to wear bikini was called greatest actress ever, later isolated herself, died alone, her body was..![submenu-img]() This film had no superstars, got slow start at box office, was made with budget of only Rs 60 lakh, earned Rs...
This film had no superstars, got slow start at box office, was made with budget of only Rs 60 lakh, earned Rs...![submenu-img]() Salman Khan to return as host of Bigg Boss OTT 3? Deleted post from production house confuses fans
Salman Khan to return as host of Bigg Boss OTT 3? Deleted post from production house confuses fans![submenu-img]() Manoj Bajpayee talks Silence 2, decodes what makes a character iconic: 'It should be something that...' | Exclusive
Manoj Bajpayee talks Silence 2, decodes what makes a character iconic: 'It should be something that...' | Exclusive![submenu-img]() Meet star, once TV's highest-paid actress, who debuted with Aishwarya Rai, fought depression after flops; is now...
Meet star, once TV's highest-paid actress, who debuted with Aishwarya Rai, fought depression after flops; is now... ![submenu-img]() IPL 2024: Jos Buttler's century power RR to 2-wicket win over KKR
IPL 2024: Jos Buttler's century power RR to 2-wicket win over KKR![submenu-img]() GT vs DC, IPL 2024: Predicted playing XI, live streaming details, weather and pitch report
GT vs DC, IPL 2024: Predicted playing XI, live streaming details, weather and pitch report![submenu-img]() GT vs DC IPL 2024 Dream11 prediction: Fantasy cricket tips for Gujarat Titans vs Delhi Capitals
GT vs DC IPL 2024 Dream11 prediction: Fantasy cricket tips for Gujarat Titans vs Delhi Capitals![submenu-img]() 'I went to...': Glenn Maxwell reveals why he was left out of RCB vs SRH clash
'I went to...': Glenn Maxwell reveals why he was left out of RCB vs SRH clash![submenu-img]() IPL 2024: Travis Head, Heinrich Klaasen power SRH to 25 run win over RCB
IPL 2024: Travis Head, Heinrich Klaasen power SRH to 25 run win over RCB![submenu-img]() Shocking details about 'Death Valley', one of the world's hottest places
Shocking details about 'Death Valley', one of the world's hottest places![submenu-img]() Aditya Srivastava's first reaction after UPSC CSE 2023 result goes viral, watch video here
Aditya Srivastava's first reaction after UPSC CSE 2023 result goes viral, watch video here![submenu-img]() Watch viral video: Isha Ambani, Shloka Mehta, Anant Ambani spotted at Janhvi Kapoor's home
Watch viral video: Isha Ambani, Shloka Mehta, Anant Ambani spotted at Janhvi Kapoor's home![submenu-img]() This diety holds special significance for Mukesh Ambani, Nita Ambani, Isha Ambani, Akash, Anant , it is located in...
This diety holds special significance for Mukesh Ambani, Nita Ambani, Isha Ambani, Akash, Anant , it is located in...![submenu-img]() Swiggy delivery partner steals Nike shoes kept outside flat, netizens react, watch viral video
Swiggy delivery partner steals Nike shoes kept outside flat, netizens react, watch viral video

































)




)
)
)
)
)
)