How do you tell the parents of a four-year-old that their daughter might be blind for the rest of her life?
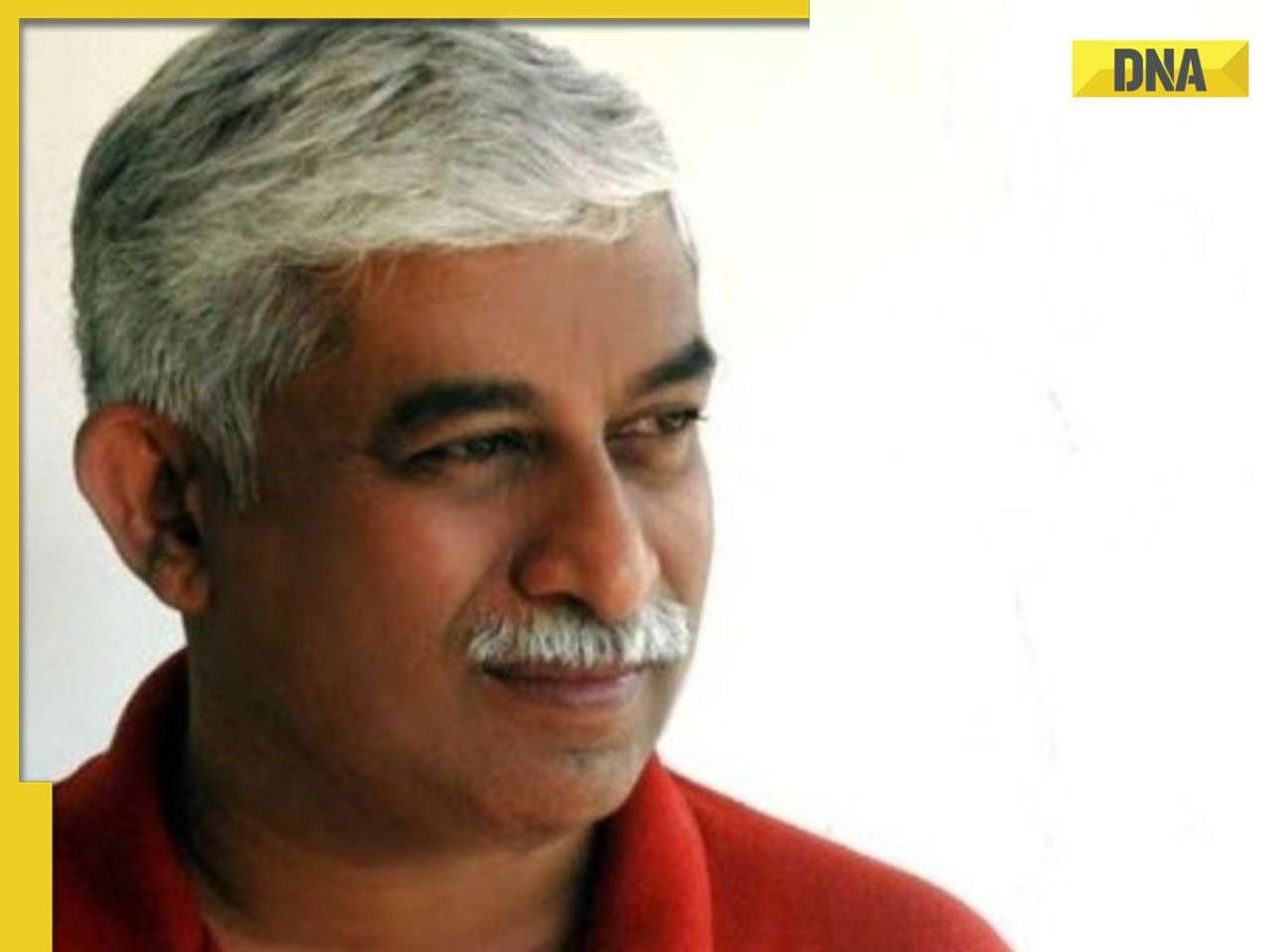
“This fair-complexioned, sweet-looking little Punjabi kid looks around, probably wondering why a group of doctors are staring at her. She obviously didn’t understand the significance of what we were saying,” says Dr Dhairyasheel Savant, surgical oncologist at SL Raheja and Saifee hospitals in Mumbai, who was one of the doctors in that group 14 years ago. Dr Savant was just starting out in oncology and this girl was one of his first few cases.
“The worst part of it was telling the parents that their daughter had a retinoblastoma, a cancerous tumour in the retina of the eye,” says Dr Savant. “It gave us all sleepless nights to think of that innocent little child who did not deserve to lose her eyesight.”
According to Dr Siddhartha Mukherjee, oncologist at the Columbia University, US, and winner of this year’s Pulitzer Prize for his book Emperor Of All Maladies: A Biography Of Cancer, oncology is a dismal discipline. But his work does not make him feel dispirited.
“Being an oncologist means that you get to sit in at a moment of another person’s life that is so hyper-acute, and not just because they’re medically ill. It’s also a moment of hope and expectation and concern,” he was quoted as saying.
Doctors deal with life and death every day. But unlike other medical specialities, oncologists have to deal with a disease as well as the sense of despair that surrounds it.
On signing a death warrant
Despite advances in medicine, a cancer diagnosis is shrouded in ambiguity. Oncologists get patients who are afraid of cancer more than almost any other disease. “A person will much more readily accept a diagnosis of diabetes than one of cancer, even if the cancer can be treated,” says Dr Vijay Haribhakti, surgical oncologist at Jaslok, Breach Candy, and Saifee hospitals. “Families asking me not to tell the patient s/he has cancer is more the rule than the exception. Even medical professionals who happen to be cancer patients make promises like ‘I’ll tell people about it when I’ve been cancer-free for five years’, but they never do.” It’s frustrating, he says, because spreading awareness is what can lead to better cancer prevention.
Sometimes, oncologists have to play God. Dr Savant recently had a patient with just a few months left to live. “All I could say to him was: I’m doing the best I can and I need your support to help fight this disease. At this point, it was time to get the family involved. Sometimes, it is not worth it to try and prolong a patient’s life. If they’re old and the cancer has spread, treatment will only help increase lifespan by a few weeks, not restore the quality of life. Whether or not to continue treatment is a call we have to take. This is never an easy choice,” says Dr Savant. “Being an oncologist, it causes me a lot of heartache to have to admit that I am honestly helpless and that except for making the patient comfortable, there’s nothing more that I can do.”
Dr Suresh Advani, oncologist at SL Raheja, Jaslok and Breach Candy hospitals, tries to deal with it in his own way. “We can never tell a patient that they have only a few months left to live. Nobody in the world is ever ready for that information. But talking positively helps, even if there’s only a small chance that the patient may survive. Patients and their families sometimes know that we’re beating around the bush, but they welcome that positivity anyway. A reaction like a smile or a joke is very encouraging for us as doctors.”
Promising new treatments
Advances in treatments, however, are making a huge difference to how oncologists look at cancer. It is no longer a gigantic, unknown and scary disease. But a decade ago, a cancer diagnosis meant doom. “We couldn’t offer the same treatments to an elderly patient as we did to a 20-year-old. Eight years back, when I was training in medical oncology, we had to turn away an 80-year-old patient because the drugs were too toxic for his age,” says Dr Indu Ambulkar, medical oncologist at SL Raheja hospital, pointing out how helpless this made her feel.
“But today, new drugs have lesser toxicity and better efficacy and can be given with positive results to even an aged patient. Targeted treatments (a process that blocks the growth of cancer cells by targeting the molecules needed for this growth) can now be offered to patients regardless of their age,” she adds.
Doctors now look at cancer like any other big challenge. “Sure, as doctors, there’s that initial ‘why me?’ question we have to answer. Then there are questions like ‘what are the survival rates?’ I could give statistics like 20% and 50%, but that doesn’t mean anything to the patient, so I tell them that there’s a 100% or a 0% chance they’ll survive depending on whether they decide to fight. But after that, things get better. The attitude to cancer has changed and patients know they have to fight the cancer regardless of the odds,” says Dr Savant, who has seen the attitude to cancer shift over the last 14 years.
‘Fascinating to watch patients heal’
But cancer is still relatively unknown when compared with other diseases. So there’s greater team-work involved. “I have to consult with radiologists and medical oncologists on what course of treatment we should take,” says Dr Haribhakti. “Sometimes, patients go for less expensive treatments to doctors who don’t really have the expertise in reconstruction surgery. It’s terrible to see a patient suffer because of that.”
Awareness, he says, is the only way people can avoid late diagnoses and botched surgeries. This awareness will come when the stigma around cancer is completely lifted. “Like Dr Siddhartha Mukherjee said, ‘I’m happy to have won a Pulitzer, but the real prize will be if the book helps de-stigmatise the disease.’ I think that would give us oncologists a lot of joy,” says Dr Haribhakti.
“It’s a race without a finish line and that’s what makes it fascinating for me as a doctor. Oncology as a subject itself is fascinating. There’s so much scope for research and development of new drugs. But the most fascinating part of the job is to watch — and be part of — the healing process in a patient who had lost all hope,” he says.
For Dr Advani, every patient reminds him of how lucky he is. “I’m 63 years old and I am well. I see patients who are 20, newly-wed, and with their whole lives ahead of them who are dying of cancer. And when they do, their families too die a little. It’s heartbreaking. But I can’t help feeling grateful that I have been given an opportunity to live.”
![submenu-img]() Meet IIT graduate who designed EVM, worked with Microsoft and Google, he works as…
Meet IIT graduate who designed EVM, worked with Microsoft and Google, he works as…![submenu-img]() Tata Motors planning Rs 8360 crore plant to make luxury cars in India, to set up…
Tata Motors planning Rs 8360 crore plant to make luxury cars in India, to set up…![submenu-img]() Meet man who has bought most expensive property on Bengaluru's 'Billionaire Street', Sudha Murty also...
Meet man who has bought most expensive property on Bengaluru's 'Billionaire Street', Sudha Murty also...![submenu-img]() Israel-Iran news live: Israel conducts air strike in Iran in retaliation to missile attack, says report
Israel-Iran news live: Israel conducts air strike in Iran in retaliation to missile attack, says report![submenu-img]() Neeru Bajwa says Punjabi film industry lacks professionalism: ‘We are not going anywhere until…’
Neeru Bajwa says Punjabi film industry lacks professionalism: ‘We are not going anywhere until…’![submenu-img]() DNA Verified: Is CAA an anti-Muslim law? Centre terms news report as 'misleading'
DNA Verified: Is CAA an anti-Muslim law? Centre terms news report as 'misleading'![submenu-img]() DNA Verified: Lok Sabha Elections 2024 to be held on April 19? Know truth behind viral message
DNA Verified: Lok Sabha Elections 2024 to be held on April 19? Know truth behind viral message![submenu-img]() DNA Verified: Modi govt giving students free laptops under 'One Student One Laptop' scheme? Know truth here
DNA Verified: Modi govt giving students free laptops under 'One Student One Laptop' scheme? Know truth here![submenu-img]() DNA Verified: Shah Rukh Khan denies reports of his role in release of India's naval officers from Qatar
DNA Verified: Shah Rukh Khan denies reports of his role in release of India's naval officers from Qatar![submenu-img]() DNA Verified: Is govt providing Rs 1.6 lakh benefit to girls under PM Ladli Laxmi Yojana? Know truth
DNA Verified: Is govt providing Rs 1.6 lakh benefit to girls under PM Ladli Laxmi Yojana? Know truth![submenu-img]() Remember Sana Saeed? SRK's daughter in Kuch Kuch Hota Hai, here's how she looks after 26 years, she's dating..
Remember Sana Saeed? SRK's daughter in Kuch Kuch Hota Hai, here's how she looks after 26 years, she's dating..![submenu-img]() In pics: Rajinikanth, Kamal Haasan, Mani Ratnam, Suriya attend S Shankar's daughter Aishwarya's star-studded wedding
In pics: Rajinikanth, Kamal Haasan, Mani Ratnam, Suriya attend S Shankar's daughter Aishwarya's star-studded wedding![submenu-img]() In pics: Sanya Malhotra attends opening of school for neurodivergent individuals to mark World Autism Month
In pics: Sanya Malhotra attends opening of school for neurodivergent individuals to mark World Autism Month![submenu-img]() Remember Jibraan Khan? Shah Rukh's son in Kabhi Khushi Kabhie Gham, who worked in Brahmastra; here’s how he looks now
Remember Jibraan Khan? Shah Rukh's son in Kabhi Khushi Kabhie Gham, who worked in Brahmastra; here’s how he looks now![submenu-img]() From Bade Miyan Chote Miyan to Aavesham: Indian movies to watch in theatres this weekend
From Bade Miyan Chote Miyan to Aavesham: Indian movies to watch in theatres this weekend ![submenu-img]() DNA Explainer: What is cloud seeding which is blamed for wreaking havoc in Dubai?
DNA Explainer: What is cloud seeding which is blamed for wreaking havoc in Dubai?![submenu-img]() DNA Explainer: What is Israel's Arrow-3 defence system used to intercept Iran's missile attack?
DNA Explainer: What is Israel's Arrow-3 defence system used to intercept Iran's missile attack?![submenu-img]() DNA Explainer: How Iranian projectiles failed to breach iron-clad Israeli air defence
DNA Explainer: How Iranian projectiles failed to breach iron-clad Israeli air defence![submenu-img]() DNA Explainer: What is India's stand amid Iran-Israel conflict?
DNA Explainer: What is India's stand amid Iran-Israel conflict?![submenu-img]() DNA Explainer: Why Iran attacked Israel with hundreds of drones, missiles
DNA Explainer: Why Iran attacked Israel with hundreds of drones, missiles![submenu-img]() Neeru Bajwa says Punjabi film industry lacks professionalism: ‘We are not going anywhere until…’
Neeru Bajwa says Punjabi film industry lacks professionalism: ‘We are not going anywhere until…’![submenu-img]() Meet actress who married a CM against her family's wishes, became his second wife, her net worth is..
Meet actress who married a CM against her family's wishes, became his second wife, her net worth is..![submenu-img]() Meet India's richest actress, who started career with two flops, was removed from multiple films, is now worth...
Meet India's richest actress, who started career with two flops, was removed from multiple films, is now worth...![submenu-img]() Meet hit director's niece, who was bullied for 15 years, Bollywood debut flopped, will now star in Rs 200 crore project
Meet hit director's niece, who was bullied for 15 years, Bollywood debut flopped, will now star in Rs 200 crore project![submenu-img]() Abhilash Thapliyal discusses Maidaan, reveals he lost chance to play PK Banerjee in Ajay Devgn's film for this reason
Abhilash Thapliyal discusses Maidaan, reveals he lost chance to play PK Banerjee in Ajay Devgn's film for this reason![submenu-img]() IPL 2024: Ashutosh Sharma's heroics in vain as Mumbai Indians return to winning ways with 9-run victory over PBKS
IPL 2024: Ashutosh Sharma's heroics in vain as Mumbai Indians return to winning ways with 9-run victory over PBKS![submenu-img]() LSG vs CSK, IPL 2024: Predicted playing XI, live streaming details, weather and pitch report
LSG vs CSK, IPL 2024: Predicted playing XI, live streaming details, weather and pitch report![submenu-img]() LSG vs CSK IPL 2024 Dream11 prediction: Fantasy cricket tips for Lucknow Super Giants vs Chennai Super Kings
LSG vs CSK IPL 2024 Dream11 prediction: Fantasy cricket tips for Lucknow Super Giants vs Chennai Super Kings![submenu-img]() PBKS vs MI IPL 2024: Rohit Sharma equals MS Dhoni's massive record, becomes 2nd player to....
PBKS vs MI IPL 2024: Rohit Sharma equals MS Dhoni's massive record, becomes 2nd player to....![submenu-img]() Major setback for CSK as star player ruled out of IPL 2024, replacement announced
Major setback for CSK as star player ruled out of IPL 2024, replacement announced![submenu-img]() Canada's biggest heist: Two Indian-origin men among six arrested for Rs 1300 crore cash, gold theft
Canada's biggest heist: Two Indian-origin men among six arrested for Rs 1300 crore cash, gold theft![submenu-img]() Donuru Ananya Reddy, who secured AIR 3 in UPSC CSE 2023, calls Virat Kohli her inspiration, says…
Donuru Ananya Reddy, who secured AIR 3 in UPSC CSE 2023, calls Virat Kohli her inspiration, says…![submenu-img]() Nestle getting children addicted to sugar, Cerelac contains 3 grams of sugar per serving in India but not in…
Nestle getting children addicted to sugar, Cerelac contains 3 grams of sugar per serving in India but not in…![submenu-img]() Viral video: Woman enters crowded Delhi bus wearing bikini, makes obscene gesture at passenger, watch
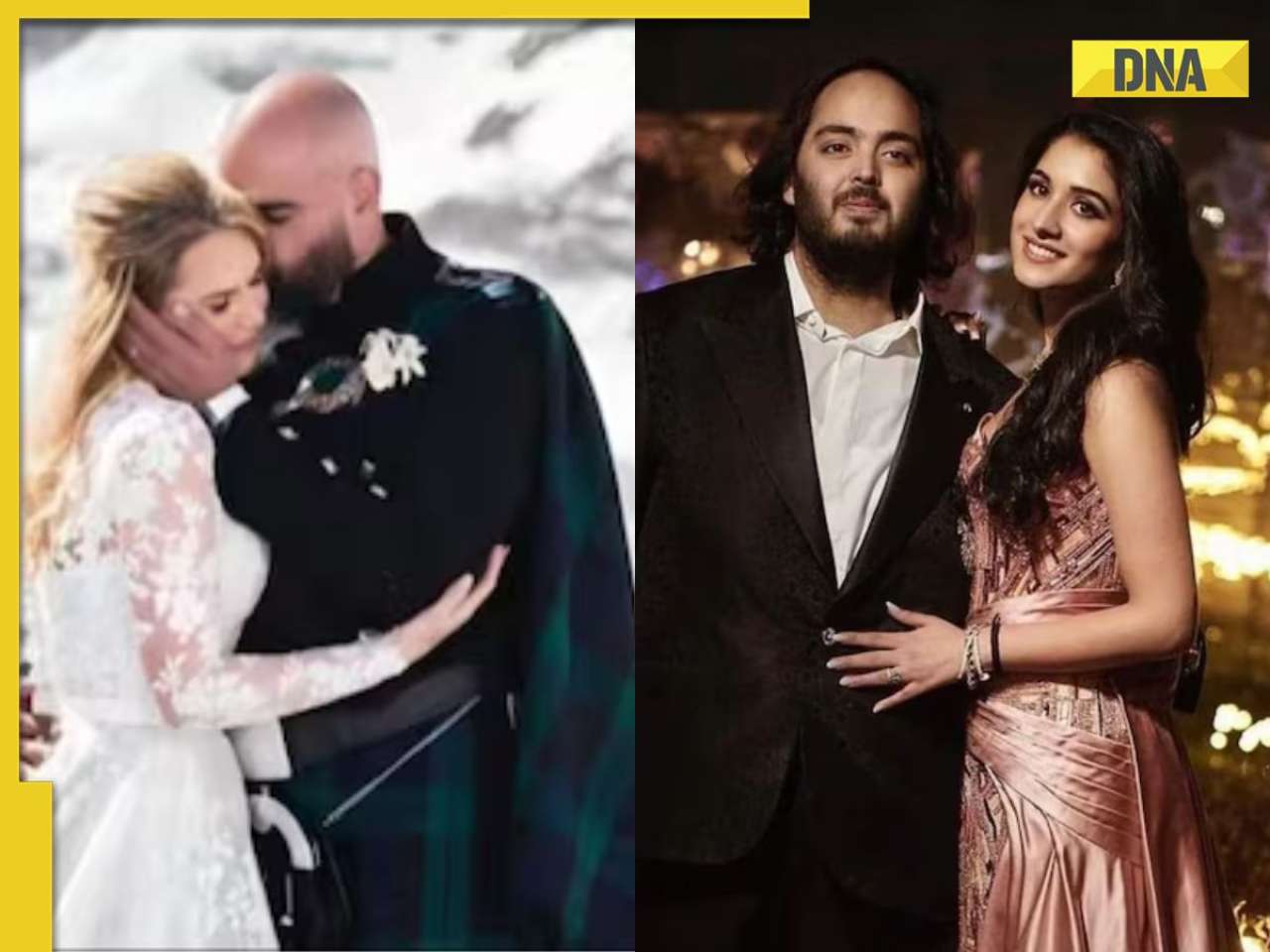
Viral video: Woman enters crowded Delhi bus wearing bikini, makes obscene gesture at passenger, watch![submenu-img]() This Swiss Alps wedding outshine Mukesh Ambani's son Anant Ambani's Jamnagar pre-wedding gala
This Swiss Alps wedding outshine Mukesh Ambani's son Anant Ambani's Jamnagar pre-wedding gala











































)
)
)
)
)
)